Abstract
It is important to prioritize screening and surveillance for neurodevelopmental dysfunction in children with SCD because this vulnerable population is at higher risk for neurological complications including stroke, silent cerebral infarction, and neurodevelopmental disorders (NDD) such as language disorders, attention deficit hyperactivity disorder, and autism spectrum disorder (ASD). The American Society of Hematology (ASH) and American Academy of Pediatrics (AAP) have published guidelines to accomplish this, as well as to improve quality of life for people with SCD and NDDs. Despite the recognition of the increased risk and the clinical guidelines, the co-occurrence rates of SCD and NDD remain lower than expected.
We hypothesize that the risk of NDDs is lower than expected in children with SCD due to low rates of neurodevelopmental screening and surveillance among primary care providers and hematologists, particularly in young children. Therefore, we examined the frequency of neurodevelopmental screening and surveillance among young children with SCD and identified clinical characteristics of young children with SCD who did not receive appropriate neurodevelopmental screening and surveillance.
We conducted a retrospective chart review using the clinic rosters of two affiliated inner-city hospitals with a pediatric hematology clinic and sickle cell neurodevelopmental clinic. Children under 5 years old with SCD confirmed by their hematologists who were not adopted or in foster care were included in the study. A total of 276 patients were identified and reviewed. NDD and ASD specific screenings were documented at the time of review, although participants may have been diagnosed later in life. Analyses were completed using chi squared test, Fisher exact test, t-test in Stata IC-15.
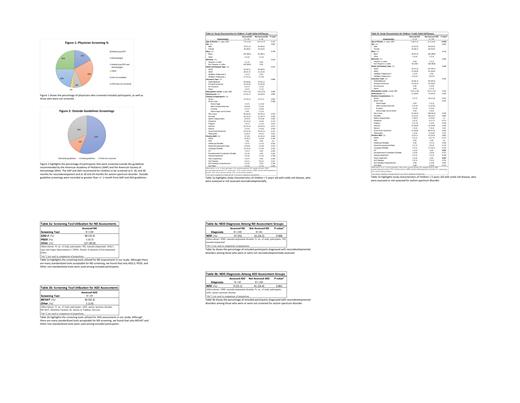
Patients were screened by a variety of providers, most commonly pediatricians and hematologists (see Figure 1). Table 1a shows the characteristics of the SCD patients assessed/not assessed for appropriate neurodevelopment (ND) by their pediatrician and/or hematologist. A total of 214 participants qualified for study inclusion and 148 participants (70%) were assessed for neurodevelopment. Ages and Stages Questionnaire- 3 (32%) and other non-standardized screening tools (85%) were the most common tool used (see Table 2a). Of the ND assessed patients (N=148), 37 (25%) were diagnosed with NDDs (see Table 3a). Among the not assessed ND patients (N=66), 16 (24%) were diagnosed with NDDs. Table 1b shows the characteristics of the SCD patients assessed/not assessed specifically for ASD by their pediatrician and/or hematologist. A total of 207 participants qualified for study inclusion and 39 participants (19%) were assessed for ASD. Modified Checklist for Autism in Toddlers (92%) was the most utilized screening tool (see Table 2b). None of these patients had ASD. Of the ASD assessed patients (N=39), 9 (23%) were diagnosed with NDDs (see Table 3a). Among the not assessed ASD patients (N=168), 41 (24%) were diagnosed with NDDs.
Children with SCD are being screened by their healthcare providers at a much lower rate than the general pediatric population. More specifically, many children with SCD were being screened for NDD, but not ASD. Among screened children, a majority were screened with non-standardized (or poorly documented) tools or outside the age guidelines recommended by ASH and AAP (see Figure 2). Children among ND and ASD assessment groups exhibited similar percentages of NDD diagnosis, which may highlight disparities in screening and early detection of these disorders; NDDs may have also been diagnosed later in life these patients. Guidelines regarding developmental screening in pediatric SCD were released in mid-2020; given the short timeline, we did not expect to see changes in practice from this chart review. However, the AAP has guidelines for developmental surveillance and screening since 2004. Due to study design, limitations include lack of access to some data at the time of review, as patient medical records were switched to another electronic system. Additionally, standardized tools may have been used but not documented in patient charts.
In conclusion, it is crucial to know the utility of these assessments in this vulnerable population. A future study could examine how the rates of screening and surveillance have changed since the guidelines release, using these data for comparison purposes.
Casella: Mast Pharmaceuticals (previously Adventrx Pharmaceuticals): Consultancy, Honoraria, Patents & Royalties. Lance: Novartis: Other: participated in research advisory board in 2020.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal